Unveiling the Connections Between Genetic Risk, Lifestyle, and Mortality: A Groundbreaking Study
In the landscape of obesity research, a recent study stands out for its innovative approach to understanding how genetics and lifestyle factors interact to influence all-cause mortality. This pioneering research sheds light on a complex relationship: while our genes may predispose us to obesity, adopting a robust healthy lifestyle can substantially mitigate associated risks, including those of mortality.
- The Genetic Risk of Obesity: A Quantitative Approach
- Methodological Innovations in Genetic Risk Assessment
- An Effective Tool for Health Professionals
- Exploring the Biological Mechanisms
- Lifestyle Factors: An Essential Component
- Real-World Applications and Considerations
- Addressing Limitations
- Implications for Future Research
The Genetic Risk of Obesity: A Quantitative Approach
At the heart of this study lies a cutting-edge model for quantifying the genetic risk of obesity, termed the Obesity Polygenic Risk Score (OPRS). Drawing data from the extensive UK Biobank cohort, researchers utilized sophisticated machine learning (ML) techniques to generate the OPRS. This method involved stacking multiple ML algorithms to capture the complex and sometimes non-linear interactions among single nucleotide polymorphisms (SNPs), which can influence obesity risk. This intricate design not only improves predictive performance but also enhances the model’s versatility, reducing the risk of overfitting—a common pitfall in predictive modeling.
Validation Across Diverse Cohorts
To ensure the reliability of the OPRS, validation was conducted using data from Nanfang Hospital, primarily involving a Chinese cohort. Interestingly, a moderate decline in the model’s performance was observed, potentially due to genetic and lifestyle disparities between European populations and their Chinese counterparts. Differences in allele frequency distributions and SNP effect sizes could contribute to this variance, alongside cultural and socioeconomic factors that might influence obesity prevalence across regions. Nonetheless, the positive correlation between OPRS and obesity phenotypes remained significant, suggesting that while genetic risks may manifest differently across populations, the underlying principles hold true.
Methodological Innovations in Genetic Risk Assessment
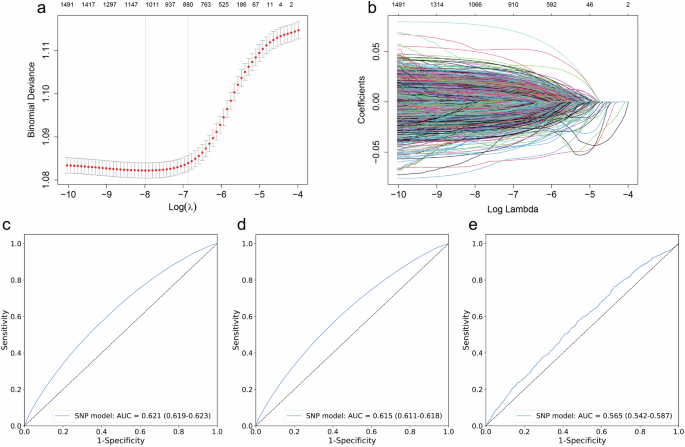
The OPRS distinguishes itself from traditional polygenic risk scores (PRS) by integrating multiple algorithms specifically designed to navigate the intricate web of genetic data. While the OPRS achieved respectable area under the curve (AUC) values—0.621 in training sets and 0.565 in external validations—its standout feature lies in its generalizability across ethnicities. Traditional PRS often exhibit biases when derived from single-ancestry populations, whereas the OPRS demonstrates applicability in diverse groups, highlighting its potential for broad clinical application.
An Effective Tool for Health Professionals
The implications of the OPRS for clinical practice are profound. By serving as a static risk indicator, health professionals can employ the OPRS as a proactive screening tool, identifying individuals at high genetic susceptibility to obesity-related health risks. This early identification enables clinicians to provide personalized recommendations for obesity management, underscoring the importance of lifestyle changes even in those with high genetic risk. Although the OPRS does require considerable computational resources for training, its efficiency during application makes it a viable option for clinical settings.
Exploring the Biological Mechanisms
Further insight into the genetic underpinnings of obesity was gained by analyzing the 508 genes that comprise the OPRS. These genes were found to be enriched in several biological processes, primarily focusing on transcriptional regulation, central nervous system function, and metabolic signaling. This aligns with previous research suggesting that obesity-related genetic variants are predominantly expressed in the central nervous system, reinforcing the significance of genetic risk in behavioral and metabolic pathways.
Lifestyle Factors: An Essential Component
Among the most noteworthy outcomes of this research is the emphasis on lifestyle factors. The study suggests that even in individuals with a high genetic risk of obesity, engaging in four specific healthy lifestyle practices can reduce all-cause mortality risks. However, it’s also crucial to recognize that those with a high OPRS still face elevated mortality risks—even if they adhere to these lifestyle guidelines. This reflects the nuanced interplay between genetic predisposition and environmental influences.
Real-World Applications and Considerations
To maximize the utility of the OPRS in clinical practice, there is an envisioned development of user-friendly platforms, possibly as a web-based calculator or integrated into Electronic Health Record (EHR) systems. Such advancements would streamline the model’s application and ensure more equitable access to genetic risk assessments. However, utmost care must be taken to ensure participant privacy and comply with regulations like the General Data Protection Regulation (GDPR). The language used in communicating risks should also empower individuals and promote positive behavioral changes rather than invoking fatalism.
Addressing Limitations
Despite the promising findings, this study is not without its limitations. Being observational in nature means that establishing causal links is challenging. Additionally, the reliance on self-reported data for lifestyle factors may introduce biases or underreporting issues. Future research should aim for more robust prospective studies that evaluate the health implications of the OPRS and incorporate culturally appropriate lifestyle assessments to broaden its applicability.
Implications for Future Research
As obesity continues to rise globally, understanding the nuanced relationship between genetics, lifestyle, and health outcomes is more critical than ever. This study not only establishes and validates a valuable model for identifying individuals at risk but also highlights the imperative role of lifestyle changes in improving health outcomes. As we move forward, further ethnic diversity in validation studies and interventional trials will be essential to fully harness the potential of the OPRS in real-world settings. Through such research, we can foster effective strategies tailored for individuals predisposed to obesity, ultimately helping to mitigate the associated mortality risks.